What is endometrial hyperplasia?
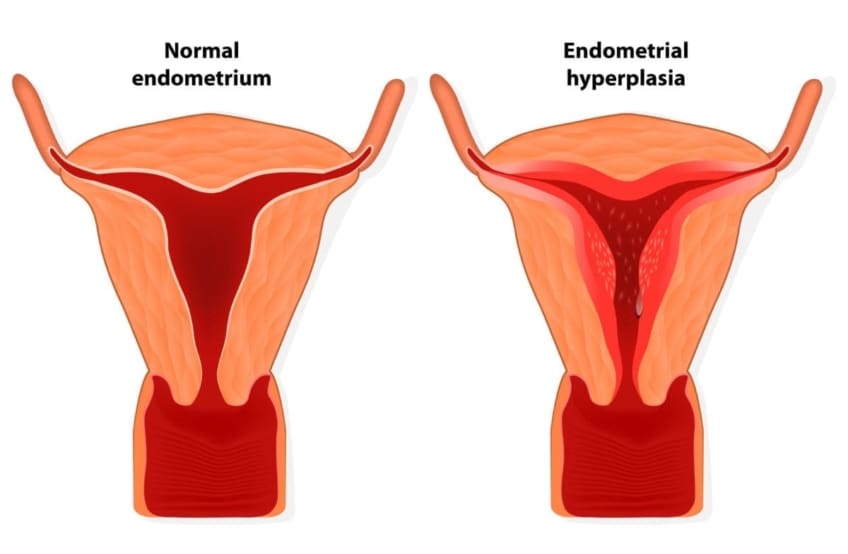
Endometrial hyperplasia is a condition in which the endometrium (lining of the uterus) is abnormally thick. There are four types of endometrial hyperplasia. These vary by the amount of abnormal cells and the presence of cell changes. The types are:
- Simple
- Complex
- Simple atypical
- Complex atypical
Symptoms
The primary symptom of endometrial hyperplasia is abnormal menstrual bleeding. Contact your doctor if you experience:
- Menstrual bleeding that is heavier or longer-lasting than usual
- Menstrual cycles (amount of time between periods) that are shorter than 21 days
- Menstrual bleeding between periods
- Not having a period (pre-menopause)
- Post-menopause bleeding
What causes of endometrial hyperplasia?
Endometrial hyperplasia is caused by too much estrogen and/or not enough progesterone. Both hormones play a role in the menstrual cycle. Estrogen makes the cells grow, while progesterone signals the shedding of the cells. A hormonal imbalance can produce too many cells or abnormal cells.
Diagnosis
Abnormal uterine bleeding can be a symptom for many things. Contact your doctor if you experience this. They can perform a physical exam and tests to diagnose the main condition. A transvaginal ultrasound measures your endometrium. It uses sound waves to see if the layer is average or too thick. A thick layer may indicate endometrial hyperplasia. Your doctor will take a biopsy of your endometrium cells to determine if cancer is present.
Prevention Tips
You cannot completely prevent endometrial hyperplasia. It is more common in people who have gone through menopause. This is because your body’s hormones and menstrual cycles change. Other risk factors for this condition include:
- Long-term use of medicines that contain high levels of estrogen or chemicals that act like estrogen
- Irregular menstrual cycles, which can be caused by infertility or polycystic ovary syndrome (PCOS)
- Obesity
- Tobacco use
- First menstrual cycle at an early age
- Menopause at an older age
- Never having been pregnant
- Family history of uterine, ovarian, or colon cancer
To help lower your risk, you can:
- Lose weight, if you have obesity
- Take progestin (synthetic progesterone), if you already are taking estrogen, due to menopause or another condition
- Take birth control or another medicine to regulate your hormones or menstrual cycle
Treatment
Treatment options for endometrial hyperplasia depend on what type you have. The most common treatment is progestin. This can be taken in several forms, including pill, shot, vaginal cream, or intrauterine device (IUD).
Atypical types of endometrial hyperplasia, especially complex, increase your risk of cancer. If you have these types, you might consider a hysterectomy. This is a surgery to remove your uterus. Your doctor will only recommend this if you no longer want to become pregnant. There are more conservative treatments for younger women who do not wish to have a hysterectomy.
Talk to your doctor who will help you decide which treatment option is best for you.
Living with endometrial hyperplasia
In most cases, endometrial hyperplasia is very treatable. Work with your doctor to create a treatment plan. If you have a severe type or if the condition is ongoing, you might need to see your doctor more often to monitor any changes.
Questions to ask your doctor
- How do I know if my bleeding is caused by endometrial hyperplasia?
- What is the most common age to get endometrial hyperplasia?
- What is my best treatment option for endometrial hyperplasia?
- What are my chances of developing cancer?
Resources
American Congress of Obstetricians and Gynecologists: Endometrial Hyperplasia
![]()
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.



