What is diabetes?
Diabetes is a disease that occurs when your body can’t properly regulate blood sugar. It happens when your body either doesn’t make or can’t use insulin properly. Insulin is a hormone that helps move glucose (sugar) from the bloodstream into cells, where it’s used for energy. When your body can’t use insulin correctly, it causes too much glucose to build up in the blood. There are two main types of diabetes.
Type 1 diabetes is an autoimmune disease, which means that it is a disorder of your immune system. A person with type 1 diabetes cannot produce insulin. Type 1 diabetes develops gradually, and it can take months or years for symptoms to show. While most diagnoses happen between the ages of 5 and 14, 1/3 of people diagnosed with type 1 are over the age of 30.
Type 2 diabetes is not an autoimmune disease and occurs when your body doesn’t produce enough insulin or doesn’t use insulin as it should. Type 2 diabetes can cause serious health problems if not managed through lifestyle changes, medication and regular monitoring.
Symptoms of diabetes
Diabetes symptoms vary from person to person. The early stages of diabetes have very few symptoms. You may not know you have the disease. But damage may already be happening to your eyes, your kidneys and your cardiovascular system. Common symptoms include:
- Extreme hunger
- Extreme thirst
- Frequent urination
- Unexplained weight loss
- Fatigue or drowsiness
- Blurry vision
- Slow-healing wounds, sores, or bruises
- Dry, itchy skin
- Tingling or numbness in the hands or feet
- Frequent or recurring skin, gum, bladder, or vaginal yeast infections
If blood sugars are extremely high, people can develop diabetic ketoacidosis (DKA). This is a very dangerous complication of uncontrolled diabetes and can lead to coma or death if left untreated. People with DKA might have:
- Nausea or vomiting more than once
- Deeper, faster breathing
- The smell of nail polish remover coming from your breath
- Weakness, drowsiness, trembling, confusion, or dizziness
- Uncoordinated muscle movement
If you suspect someone is going into DKA, seek medical attention immediately.
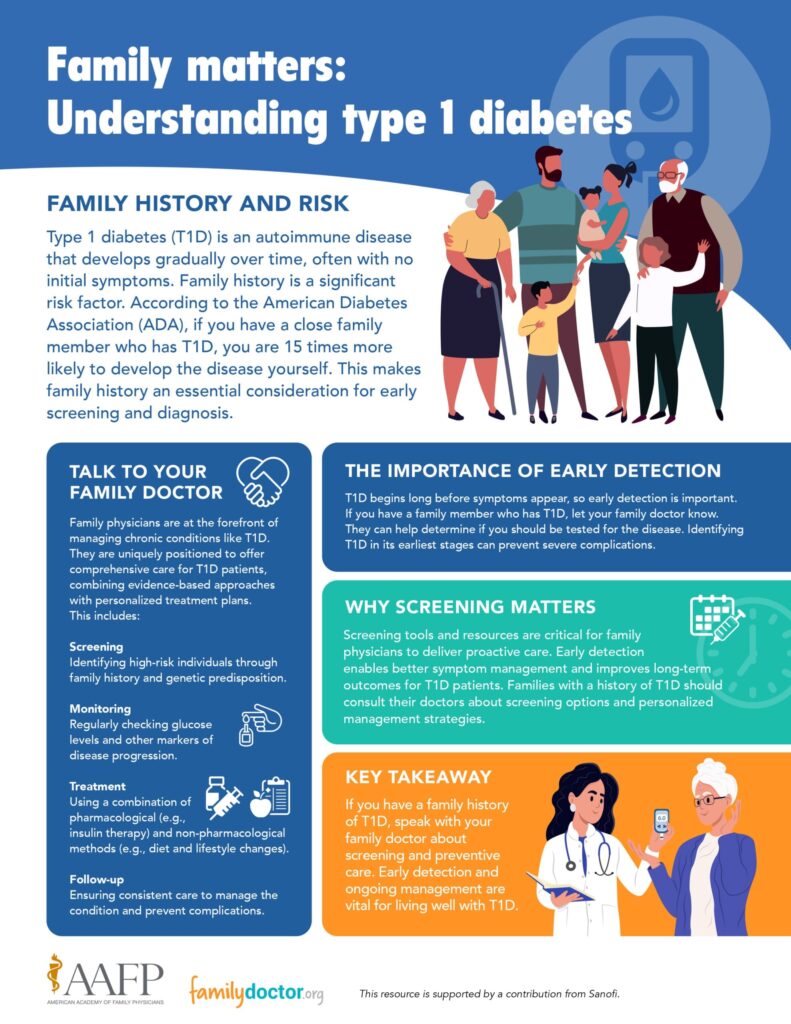
Who is at risk for type 1 diabetes?
Anybody can develop type 1 diabetes, as 85% of people diagnosed with the disease have no family history of diabetes.
However, you have a greater risk of type 1 diabetes if one of your parents or one of your siblings has it. According to the American Diabetes Association, if you have a close family member who has type 1 diabetes, you are 15 times more likely to develop the disease yourself. Tell your doctor, as they may want to test you for diabetes early.
How is type 1 diabetes diagnosed?
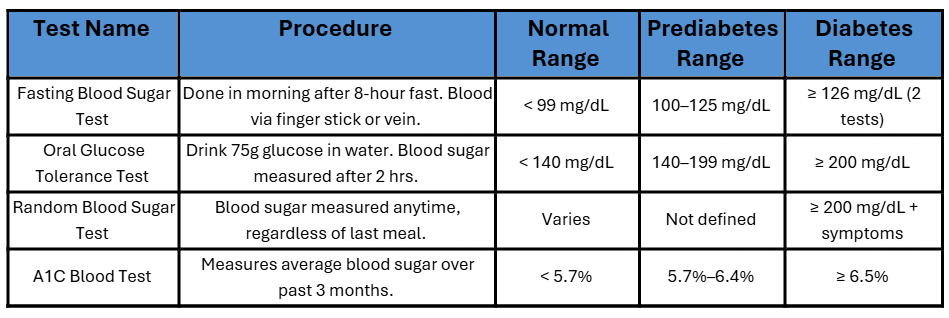
To check for diabetes, your doctor will perform one of the following tests:
- Fasting blood sugar test. This test is usually done in the morning after an 8-hour fast (not eating or drinking anything except water for 8 hours before the test). The blood test typically involves a finger stick to get a drop of blood.
- Oral glucose tolerance test. During this test, you will drink a beverage containing glucose dissolved in water. This tastes like sweet water. Two hours later, a doctor or nurse will measure the amount of glucose in your blood. Random blood sugar test. This test measures the level of glucose in your blood at any time of day. It doesn’t matter when you last ate.
- A1C blood test. This test provides information about a person’s average levels of blood glucose over the previous 3 months. The results are reported as a percentage. A normal A1C level is below 5.7%.
Can Type 1 diabetes be prevented or avoided?
Type 1 diabetes cannot be prevented or avoided. However, some new drugs have been shown to help delay type 1 diabetes in at-risk patients. Your physician will know which drugs could help you and your diagnosis.
Type 1 diabetes management
Use the free Neighborhood Navigator tool to find community support or screening options.
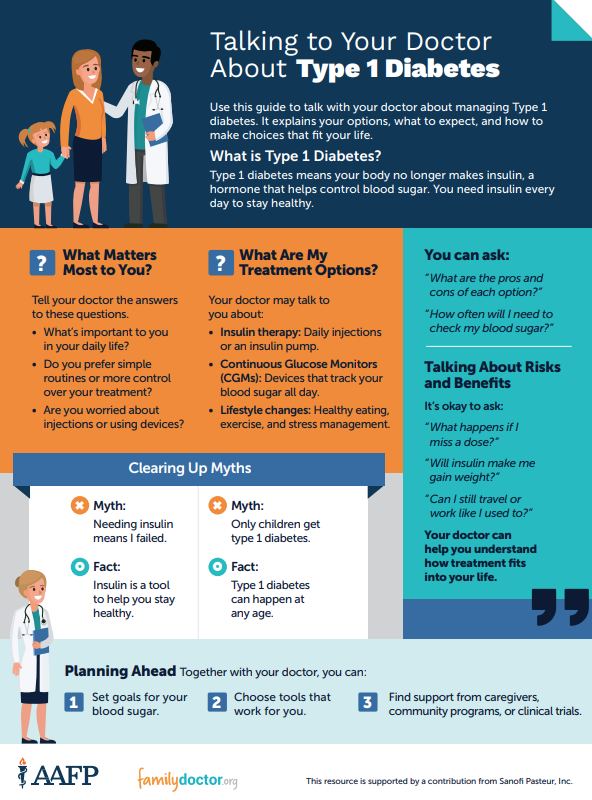
1. Take your insulin and monitor your blood sugar
Everyone with type 1 diabetes needs insulin therapy, which helps you keep your blood sugar levels in a healthy range. Insulin can be taken via injections or an insulin pump. Your doctor will help you choose the best method, timing and dosage for your needs.
You will need to use a blood glucose monitor to check blood sugar levels on your own. Continuous glucose monitors (CGM) are also an option for many.
2. Eat smart and stay consistent
Your diet plays a big role in how well the insulin works. Focus on eating whole grains, fruits, vegetables, lean proteins and healthy fats. Try to eat three meals a day at regular times, which helps keep your blood sugar steady. Avoid foods high in added sugars, unhealthy fats, and alcohol, which can cause blood sugar spikes or drops.
3. Stay active and maintain a healthy weight
Exercise helps your body use insulin more effectively and lowers blood sugar levels. It also boosts your energy, supports heart health and helps manage weight. Whether it’s walking, biking or dancing, find something you enjoy. Always talk to your doctor before starting a new routine.
Living with diabetes
You can live a normal life with well-controlled diabetes. You’ll need to make sure that your blood sugar levels stay within a normal range.

What happens if my blood sugar gets too low?
If your blood sugar gets too low, you might experience a variety of symptoms, including but not limited to:
- Fatigue
- Problems with muscle coordination
- Sweating
- Twitching
- Fainting
- Seizures
At the earliest sign of any of these symptoms, eat or drink something that will raise your blood sugar quickly. This could include candy, juice, milk or raisins. If you don’t feel better in 15 minutes or if monitoring shows that your blood sugar level is still too low, eat or drink another item to raise your blood sugar fast. Always keep a supply of these items on hand for emergencies.
What happens if my blood sugar gets too high?
You may not know if your blood sugar is too high unless you test it yourself. However, you may experience common symptoms such as:
- Frequent urination
- Extreme thirst
- Blurry vision
- Feeling tired
Some factors unrelated to food can make your blood sugar high. This includes not taking your insulin correctly, overeating at a meal, illness, having hormonal changes, and stress. If your blood sugar level is too high, you may need to take an extra dose of rapid- or short-acting insulin to return to normal. Your doctor can tell you how much insulin you need to take to lower your blood sugar level.
Questions to ask your doctor
- What type of insulin do I need, and how do I take it properly? Understanding your insulin regimen—including types, timing, and delivery method—is essential for managing blood sugar.
- How often should I check my blood sugar, and what are my target levels? Ask about using a glucose meter or continuous glucose monitor (CGM), and what to do if your levels are too high or low.
- What should I eat, and how can I plan meals to keep my blood sugar stable? A balanced diet is key. Ask for guidance or a referral to a registered dietitian or diabetes educator.
- What long-term health checks do I need (like eye, foot, and kidney exams)? Type 1 diabetes can affect many parts of the body, so regular screenings are important for prevention and early detection.
ADVERTISEMENT
ADVERTISEMENT




