What is an ectopic pregnancy?
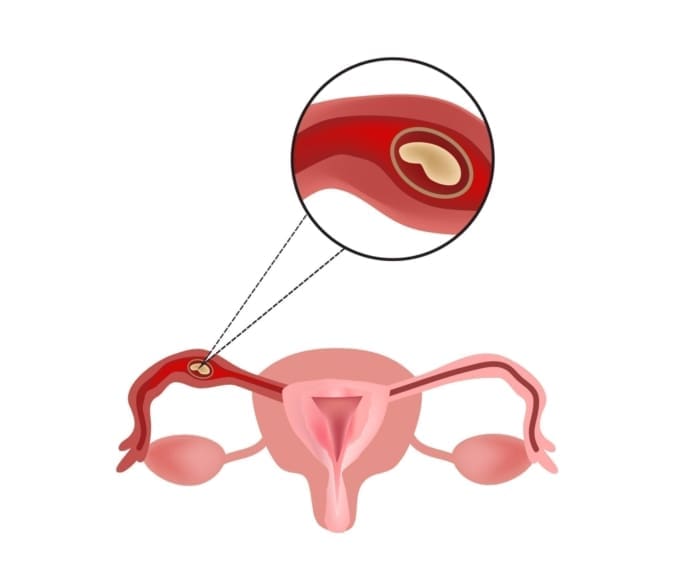
An ectopic pregnancy happens when a fertilized egg grows outside the uterus.
In a normal pregnancy, a fertilized egg implants and grows in the uterus (also called the womb). In an ectopic pregnancy, the fertilized egg doesn’t make it to the uterus. It implants somewhere else, most often in the fallopian tube. This is called a tubal pregnancy. It can also occur in the ovary, cervix, or abdomen.
An ectopic pregnancy can be dangerous for the mother. As the pregnancy grows, it could cause the organ it is implanted in to rupture (burst). This can cause major internal bleeding. That’s why it is important to find an ectopic pregnancy in its early stages.
Symptoms of an ectopic pregnancy
The early signs of an ectopic pregnancy are like those of a normal pregnancy:
- Missed periods
- Tender breasts
- Nausea
- Vomiting
- Fatigue
- Frequent urination
- A positive home pregnancy test
The first warning signs of ectopic pregnancy may include:
- Abnormal vaginal bleeding
- Low back pain
- Mild pain in the abdomen or pelvis
- Mild cramping on one side of the pelvis
If you have any of these symptoms, you should call your doctor.
As an ectopic pregnancy grows, it may rupture. Then you may experience more serious symptoms. These could include:
- Sudden, severe pain in the abdomen or pelvis
- Shoulder pain
- Feeling weak, faint, or dizzy
If you experience these symptoms, get medical help right away.
What causes an ectopic pregnancy?
Usually, an ectopic pregnancy happens because the fertilized egg couldn’t move down the fallopian tube quickly enough. An infection or inflammation in the tube can cause it to be partially or completely blocked. This is commonly caused by pelvic inflammatory disease (PID).
Another common reason tubes get blocked is endometriosis. This is when cells from the lining of the uterus grow outside the uterus. The cells can grow inside the fallopian tube and cause blockages. Scar tissue from previous abdominal surgery or fallopian tube surgery can also block the tube.
Any pregnancy can be an ectopic pregnancy. But you’re more likely to have one if you:
- Are older than 35 years of age
- Have had infections (such as pelvic inflammatory disease) or operations in the pelvic area
- Have endometriosis
- Are using assisted reproductive methods to become pregnant, such as in vitro fertilization (IVF)
- Smoke
- Have a history of inflammation of the fallopian tubes or abnormally shaped fallopian tubes
- Have had trouble getting pregnant or have had fertility treatment
- Have had an ectopic pregnancy in the past
How is an ectopic pregnancy diagnosed?
Ectopic pregnancies can be hard to diagnose because the first symptoms are the same as those of a normal pregnancy. If your doctor thinks you may have an ectopic pregnancy, they may do the following:
- Perform a pelvic exam to check the size and shape of your uterus.
- Order a urine test and a blood test to check your levels of human chorionic gonadotropin (hCG). This is a hormone that is produced by the placenta. If you have an ectopic pregnancy, you may have a low hCG level.
- Perform a transvaginal ultrasound. During this procedure, a wand is inserted into your vagina. Sound waves from the wand make pictures of organs in the body. This will allow your doctor to see where the pregnancy is growing.
Can an ectopic pregnancy be prevented or avoided?
You can’t prevent an ectopic pregnancy, but you can try to control your risk factors. Don’t smoke. If you do smoke, plan on quitting before you get pregnant. Before getting pregnant, use a condom when having sex. This can help prevent sexually transmitted infections, such as chlamydia and gonorrhea, which can cause PID.
If you’re at higher risk of having an ectopic pregnancy, talk to your doctor. They may take extra steps to detect an ectopic pregnancy early. This could include checking your hormone levels or scheduling an early sonogram.
Treatment
If a pregnancy is ectopic, the egg can’t develop. The ectopic tissue must be removed. This can be done with medicine or surgery.
If an ectopic pregnancy is discovered early, your doctor can give you a shot of medicine called methotrexate. This medicine stops cells from growing and ends the pregnancy. Your body then absorbs the ectopic tissue.
Some ectopic pregnancies require surgery. These include those that aren’t discovered early enough, or that cause a pelvic organ to rupture. Surgery is usually done with laparoscopy. This procedure uses a tiny camera that is inserted into your body through small cuts in your abdomen. Special tools are used to remove the pregnancy. If your fallopian tube or another organ has burst, your doctor may remove that, as well.
Whether you’re treated with medicine or surgery, your doctor will want to see you regularly afterward. They will monitor your hCG levels to make sure they go back to normal. This can take several weeks.
Living with an ectopic pregnancy
Whether you’re treated with medicine or surgery, your recovery may take several weeks. You may feel tired and have abdominal pain or discomfort. You also might still feel pregnant for a while. It takes a while for the hCG levels in your body to drop. It will probably take a few cycles before your periods go back to normal.
If you’ve had an ectopic pregnancy, you’re more likely to have another one. You also may have trouble getting pregnant again. You should give yourself time to heal before you try to get pregnant after having an ectopic pregnancy.
Having an ectopic pregnancy can be emotionally hard. You may feel sad, angry, and confused. Talk about your feelings with your partner, a trusted family member, or friend. Allow yourself the chance to Find a family member or friend you can talk to about your feelings. Allow yourself to grieve the loss of a pregnancy.
Questions for your doctor
- Could vaginal bleeding in early pregnancy be a sign of ectopic pregnancy?
- Where is my ectopic pregnancy located?
- What treatment do I need?
- Will I need surgery?
- I’m having a hard time dealing with my feelings. Is there someone I could talk to or a support group in my area?
- I’d like to get pregnant again. Is there anything I can do to minimize my risk of having another ectopic pregnancy?
Resources
National Institutes of Health, MedlinePlus: Ectopic Pregnancy
![]()
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.






