What is a transient ischemic attack (TIA)?
A transient ischemic attack (TIA) is a stroke. It is considered a warning stroke. During this type of stroke, blood flow to your brain is blocked for a few minutes to a few hours. The average amount of time is one minute. Most symptoms go away within 24 hours. That is far less than a major stroke. There is usually no long-term damage following a TIA. This type of stroke significantly increases your risk of a major stroke.
Symptoms of transient ischemic attack (TIA)
TIA symptoms are similar to a major stroke. They include:
- Weakness/loss of feeling in your face, arm, or leg
- Trouble seeing in one or both eyes
- Difficulty smiling or speaking
- Confusion
- Sudden, severe headache
- Difficulty walking or balancing
What causes transient ischemic attack (TIA)?
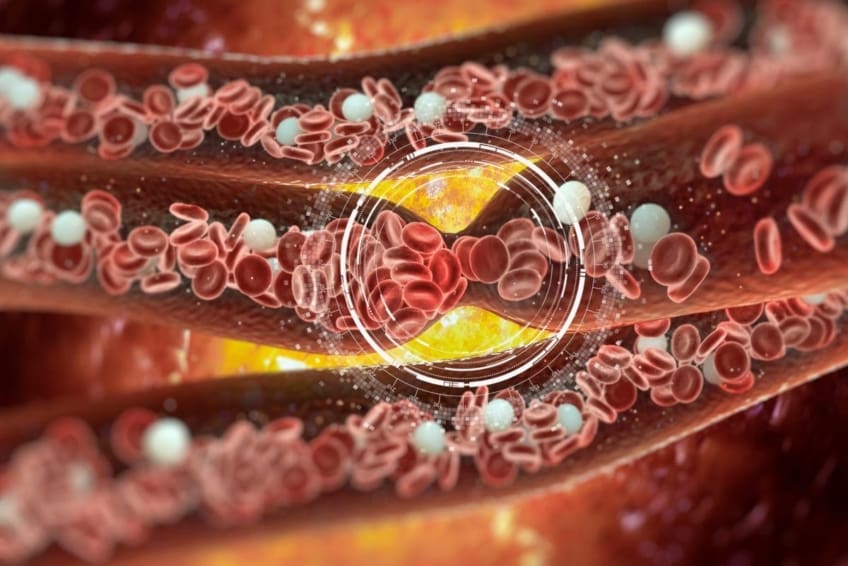
All strokes are caused by reduction or loss of blood flow. The most common cause is a blood clot. This is same for a major stroke. Blood clots are caused by cholesterol buildup. As cholesterol blocks your arteries, it forms a blood clot. Eventually, the clot breaks free. The clot travels to your brain. That’s where the TIA occurs. Managing your cholesterol levels through diet, exercise, and medicine lowers your risk.
Other medical conditions can increase your chances of having a stroke. These include high blood pressure, diabetes, and obesity. Lifestyle changes can reduce the risk of stroke. This includes not smoking and limiting alcohol. Other risks include age, heredity, gender, and ethnicity. If you’ve had one stroke, you are at a higher risk of having another one.
How is transient ischemic attack (TIA) diagnosed?
It’s difficult to identify a TIA from a major stroke as it’s happening. Self-awareness is important. Getting to a hospital or calling 911 also is important. That’s because treating a TIA or major stroke fast prevents further damage. A doctor will perform a physical exam. They will ask you about your medical history. This includes questions about other medical conditions and your lifestyle. The doctor will listen to your heart and lungs and test you for signs of numbness, weakness, or other neurologic problems.
A TIA may only last minutes but could last longer. You, a family member or friend should remember your symptoms and what time they began. All tests and exams will happen after you have the TIA.
Certain imaging tests can diagnose a stroke. They include:
- Carotid ultrasonography. This uses sound waves to examine the blood flow through your carotid arteries. These are the arteries in your neck that supply blood to your brain.
- CT (computerized tomography). A large x-ray machine will be used to take detailed internal pictures of your body.
- CTA (computerized tomography angiography). This combines a CT scan with an injection of a special dye that will help create pictures of blood vessels and tissues in your body.
- MRI (magnetic resonance imaging). Strong magnetic fields and radio waves are used to form pictures of the inside of your body.
- MRA (magnetic resonance angiography). Similar to an MRI, this test specifically looks at your blood vessels.
- TTE (transthoracic echocardiogram). In this test, ultrasound is used to create images of your heart.
- TEE (transesophageal echocardiogram). In this test, the ultrasound probe is inserted into your esophagus to take pictures of your heart. Since your esophagus and heart are next to each other in your chest, this shows details of the heart that may not be seen on a transthoracic echocardiogram
Sometimes an arteriography (a test that creates a picture of your arteries using dye and X-rays) is used to diagnose a TIA or minor stroke.
Transient ischemic attack (TIA) treatment
Most of the time, your body treats a TIA on its own. The blood clot quickly dissolves. A TIA still requires immediate attention. Go to an emergency room when you recognize symptoms. Time is critical in treating all strokes. The sooner you are treated, the better your recovery and outcome.
Treatment may include:
- Antiplatelet medicine. Antiplatelet medicines help prevent blood clots. They don’t allow certain cells in the blood (called platelets) to clump together. This reduces the risk of blockages in the arteries that can lead to heart attack and stroke. They are sometimes prescribed along with aspirin therapy.
- Anticoagulants (blood thinners). Blood thinners don’t actually thin the blood. They decrease the ability of the blood to clot. This helps prevent clots from forming in the blood vessels. It also may prevent clots from becoming larger. Large clots can cause more serious problems.
- Surgery. Surgery would open a clogged artery. You may need medicine and surgery. Endarterectomy surgery is necessary for people with a narrow neck artery. This surgery cleans blockages from that artery.
Can transient ischemic attack (TIA) be prevented or avoided?
After a TIA, your doctor may want you to take aspirin. Aspirin can help keep your blood from forming clots that block your arteries. If taking low-dose aspirin is right for you, it is important to follow your doctor’s instructions. Your doctor may also prescribe a statin. Statin drugs help to lower your cholesterol levels and avoid cholesterol buildup in your arteries.
You also can reduce risk through healthy living and managing diseases that cause strokes. Maintain a healthy diet, exercise, don’t smoke, limit alcohol, and take your medicines. This is good advice whether you are at risk or not. See your doctor if you have a medical history, family history, or other risk factors. A TIA is a warning for a future, major stroke. Without lifestyle changes and medicine, a second TIA or major stroke can happen within a year of your first TIA. Even with healthy changes, there’s no guarantee you won’t have a stroke.
Living with transient ischemic attack (TIA)
TIA’s do not cause long-term damage (walking, talking). Anxiety and worry about another stroke is common. This is true even after making lifestyle changes and taking medicine. Teach yourself, your family, and friends to recognize the signs of a stroke. The phrase FAST helps you remember the symptoms.
F — Face. You can’t smile. Your face or mouth is drooping. This is limited to one side of your face.
A — Arms. You can’t raise one or both arms.
S — Speech. You can’t speak, repeat a simple phrase. Your speech is slurred.
T — Time. Time is the most important factor in treating a stroke. Receiving treatment within 3 hours of your symptoms provides the best outcome and recovery. The sooner, the better.
Teach your family and friends the FAST rule in case you cannot communicate.
Questions to ask your doctor
- How much does family history increase your risk of stroke?
- Can medicines cause stroke?
- Can caffeine cause a stroke?
- Are there other conditions that could cause these symptoms?
- What should I do if I am more than 4.5 hours from a hospital for treatment?
- What are the complications of an untreated stroke?
- Can I die from a TIA?
Resources
American Stroke Association: Transient Ischemic Attack
Centers for Disease Control and Prevention: Stroke
National Institute of Neurological Disorders and Stroke: Transient Ischemic Attack Information Page
![]()
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.



