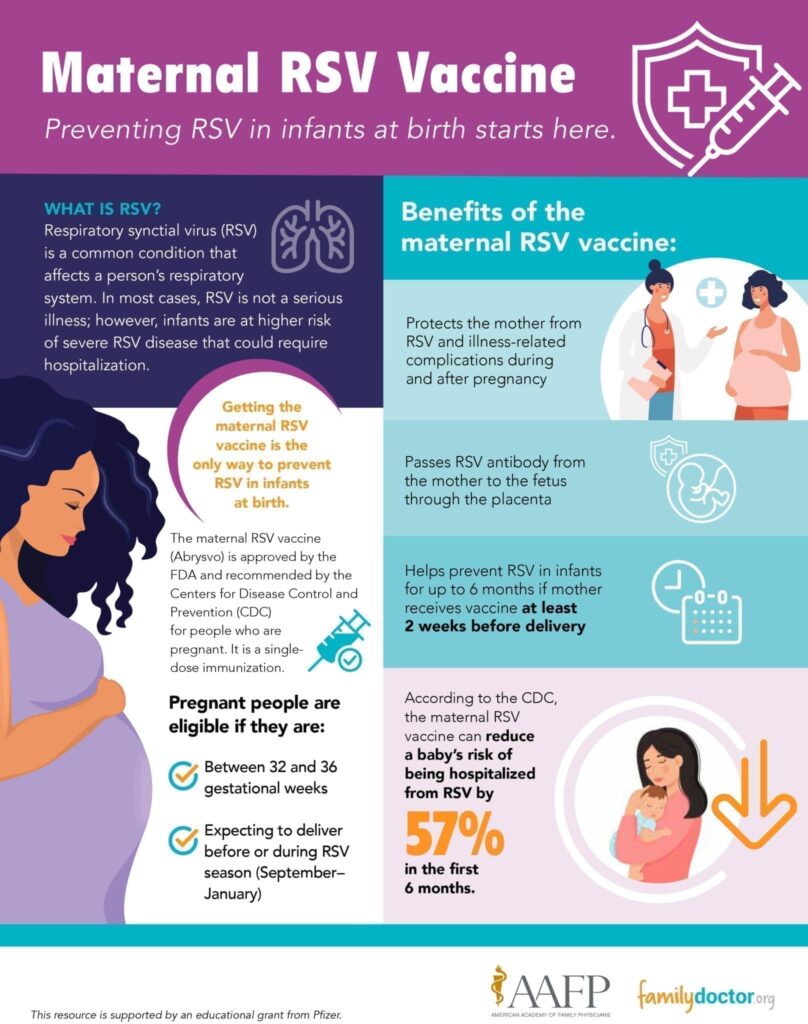
Respiratory synctial virus (RSV) is a common condition that affects a person’s respiratory system. In most cases, RSV causes mild, cold-like symptoms. However, infants and older adults are at higher risk of severe RSV disease and could require hospitalization.
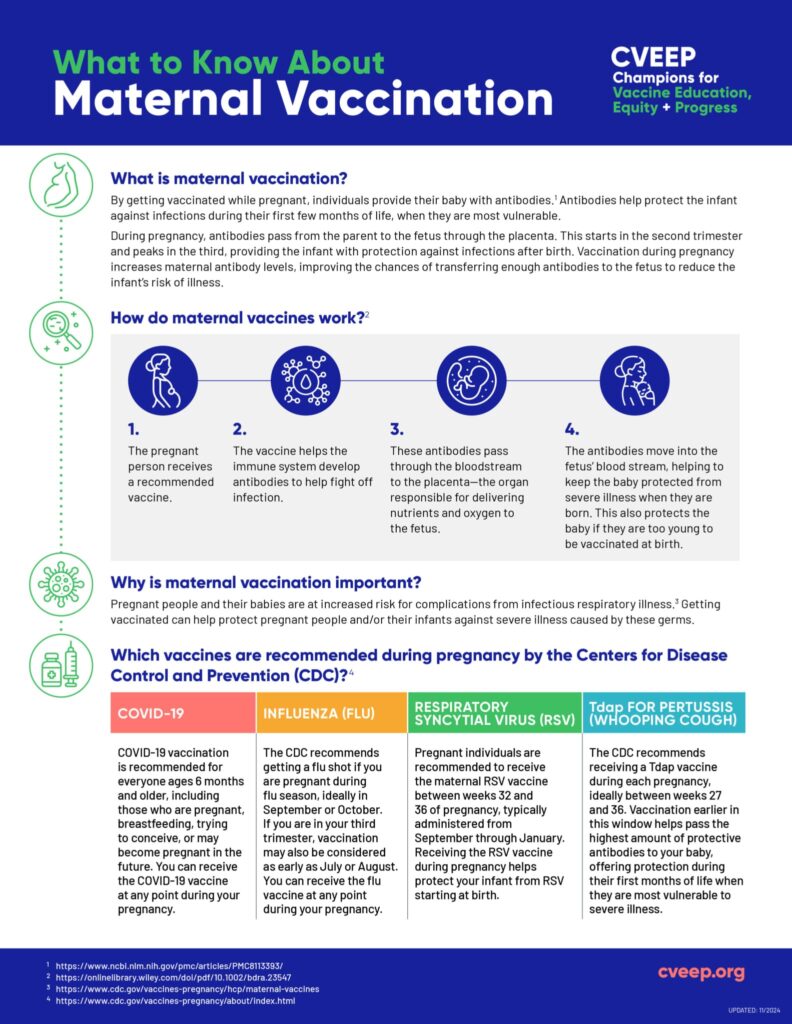
In August 2023, the U.S. Federal Drug Administration (FDA) approved the first RSV vaccine (Abrysvo) for pregnant people to help prevent severe RSV in infants. It also protects the mother from potential illness or complications. Abrysvo is recommended by the Centers for Disease Control and Prevention (CDC). Women who are between 32 and 36 weeks of pregnancy are eligible for the single-dose immunization during RSV season, which is typically September through January for most states in the continental United States.
Path to improved health
What could happen if a pregnant woman gets RSV? Can a mom give RSV to her baby?
Yes. Although symptoms from RSV are often mild, pregnant people are at greater risk of illness-related complications, such as preeclampsia or preterm labor. There is also a risk of the mother passing the virus to the fetus through the placenta.
What could happen if my baby gets RSV?
Because infants don’t have a fully developed immune system, they are vulnerable to severe illnesses such as RSV infections. In the United States, the CDC estimates that 58,000 to 80,000 children younger than 5 years old are hospitalized each year due to RSV infection. Possible complications from RSV exposure include lower birth weights and lung disease.
Can mom pass RSV antibody to baby?
Yes. If you are pregnant and receive the RSV vaccine, your body will respond to the immunization by making a protein (called an antibody) to protect against the virus that causes RSV. It takes about 2 weeks to build up the antibody, which will then be passed to the baby. The result of getting the vaccine means your newborn will be protected from RSV at birth when babies are at the highest risk.
How can I prevent RSV during pregnancy?
The only way to prevent RSV during pregnancy is to receive the maternal vaccine. The vaccine is administered as a shot (single dose) into your upper arm.
How effective is the maternal RSV vaccine?
According to the CDC, the maternal RSV vaccine can reduce a baby’s risk of being hospitalized from RSV by 57% in the first 6 months.
Things to consider
If you are pregnant and expected to give birth during peak RSV season, talk with your doctor about the benefits and risks of the maternal RSV vaccine. The most common side effects reported during clinical trials were pain at the injection site, headache, nausea, and muscle pain. Severe allergic reactions are rare but can happen.
If you are unable to get the maternal RSV vaccine, your baby may be eligible to receive the RSV immunization. Nirsevimab (Beyfortus) was approved by the FDA in July 2023 for the prevention of severe RSV disease in babies. It is typically administered for babies at birth or up to 8 months of age who are born during or preceding their first RSV season. It may also be recommended for children up to 19 months of age who are entering their second RSV season and are at increased risk for severe RSV.
According to the CDC, nirsevimab reduces the risk of severe RSV disease by about 80%. A single dose of the immunization protects infants for at least 5 months, when they are at greatest risk of RSV.
ADVERTISEMENT
ADVERTISEMENT




