
What is mitral valve prolapse?
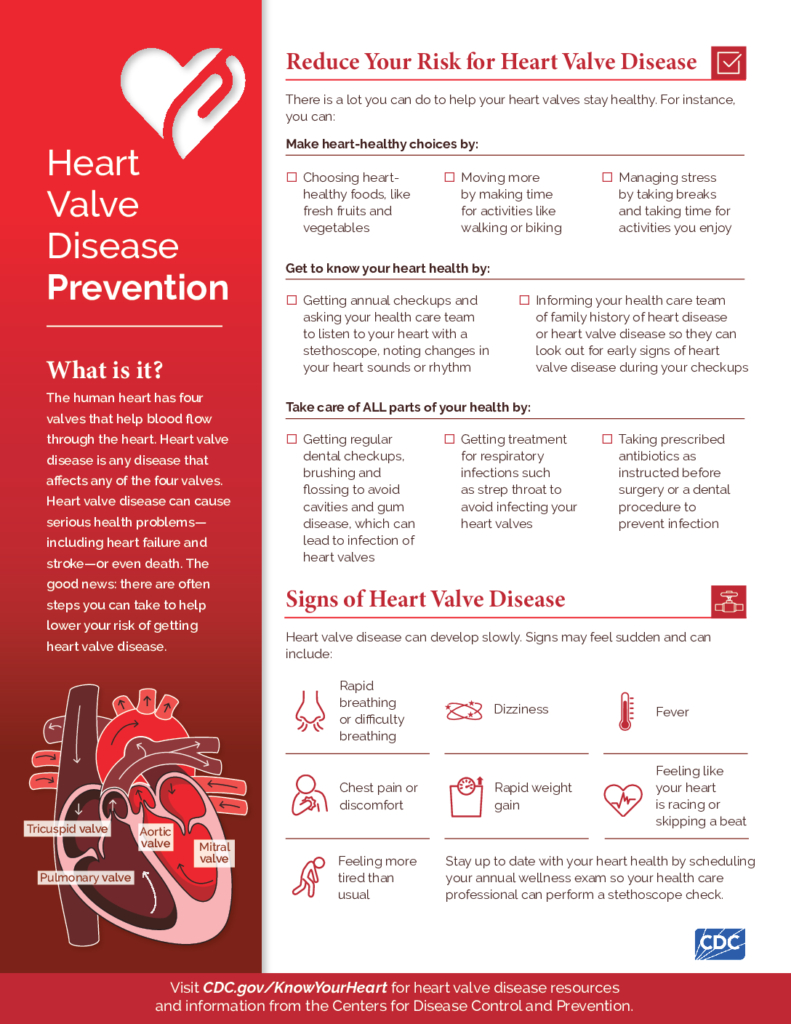
Mitral valve prolapse is a problem in your heart. Your heart has four chambers. The mitral valve controls the flow of blood between 2 of the chambers. These are the left atrium and the left ventricle. Normally, when the heart relaxes in between beats, the 2 flaps of the mitral valve swing open to let blood flow from the atrium to the ventricle. The flaps normally open only one way and the blood only flows one way.
If you have mitral valve prolapse, the flaps of the mitral valve are “floppy” and don’t close properly. Sometimes this can allow blood to leak from the ventricle back into the atrium. When this happens, you may experience symptoms.
Approximately 2% of Americans have mitral valve prolapse. More women have it than men.
Symptoms
Most people don’t know that they have mitral valve prolapse. It often causes no symptoms. If the blood leaks back into the atrium, you may have symptoms that can include:
- Feeling like your heart is racing or is skipping beats
- Chest pain that comes now and then
- Shortness of breath (sometimes worse with exertion)
- Anxiety or panic
What causes mitral valve prolapse?
Doctors don’t know the exact cause of mitral valve prolapse. People are usually born with it. It tends to run in families. You could have a higher risk of mitral valve prolapse if you have certain conditions, including:
- Connective tissue disorders (Marfan or Ehlers-Danlos syndrome)
- Graves’ disease
- Skeletal problems, such as scoliosis
- Muscular dystrophy
- History of rheumatic fever
Aging also raises your risk.
How is mitral valve prolapse diagnosed?
Usually, your doctor will find mitral valve prolapse during a regular exam. When listening to your heart with a stethoscope, your doctor may hear the flap of your mitral valve make a clicking sound. If blood is flowing back into the atrium, your doctor will hear a “whooshing” sound. This sound is called a murmur.
To find out how well your valve is working, your doctor may order an echocardiogram. This provides a picture of your heart that shows your valve as the blood flows through it. This can help your doctor decide if you need treatment. Other tests that can help diagnose mitral valve prolapse include a chest X-ray or an EKG.
Can mitral valve prolapse be prevented or avoided?
There is nothing you can do to prevent or avoid mitral valve prolapse. Most people are born with it.
One complication from mitral valve prolapse is called infective endocarditis (IE). This is an infection in your heart. If you have mitral valve prolapse, antibiotics can prevent you from getting IE. If you’re at high risk of getting IE, you can take antibiotics before surgeries or dental work to avoid getting the infection. Talk to your doctor about the risks vs. benefits of taking antibiotics to prevent IE.
Treatment
Most people who have mitral valve prolapse don’t need any treatment. Only about 2 of every 100 people who have this condition have complications. Your doctor will tell you if you need treatment.
Some people who have mitral valve prolapse must limit participation in competitive sports. If your mitral valve prolapse causes chest pain or other symptoms, your doctor might prescribe medicines such as beta blockers to make your symptoms better. If your symptoms are more significant, your doctor could prescribe other medicines, such as:
- Blood thinners to reduce the risk of blood clots
- Diuretics to remove excess fluid
- Heart rhythm medicines to regulate your heart rhythm
- Vasodilators to widen your blood vessels and reduce your heart’s workload
Some people may need surgery to fix the problem. This could happen if your valve is very abnormal, or if a lot of blood is flowing in the wrong direction. Your doctor will operate to repair or replace the mitral valve.
Living with mitral valve prolapse
Most people with mitral valve prolapse can lead normal, active lives. They don’t have symptoms and don’t need treatment. If you do have symptoms, they can normally be controlled with medicine.
If you have mitral valve prolapse, you do need ongoing care. You should have follow-up visits with your doctor and monitor your symptoms. Always take your prescribed medicine. Call your doctor if your symptoms increase or get worse. It’s also a good idea to make heart-healthy lifestyle changes. These include:
- Eating a healthy diet
- Exercising regularly
- Quitting smoking
- Getting enough sleep
- Managing stress
Questions to ask your doctor
- How did I get mitral valve prolapse? Was I born with it?
- Is it life threatening?
- Do I need to make any changes to my lifestyle, such as diet or exercise?
- What are some symptoms that would indicate my condition is getting worse?
- Am I at risk for bacterial endocarditis?
- If so, what kind of medical or dental procedures put me at risk for infection?
- Will I need antibiotics before I have one of these procedures?
Resources
CDC resources on heart valve disease:
Heart Valve Disease Prevention
Discussing Your Risk and Symptoms
After a Heart Valve Disease Diagnosis

![]()
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.








